My final guest of Season Three, Joanna Strober, was the very first guest on the Subscription Stories podcast. Back then, we were talking about Kurbo, the children’s service for WW (that’s Weight Watchers new name). Today, she’s back to talk about her latest venture in direct-to-consumer healthcare, Midi Health. While Kurbo focused on helping kids get to and maintain a healthy weight, Midi is for women at midlife, helping them get better as they get older. You may have noticed my interest in how the way we stay healthy is changing—with guests from Whoop, 30 Madison, Strava, just this season alone. I am fascinated by all of the transformation in the space, as healthcare embraces the concept of a forever transaction. After all, what forever promise is more compelling than more happy, healthy minutes. Healthcare is just embarking on a massive rethinking of how to better align their business models with patient outcomes. Midi is a great example of this. In today’s talk, we cover the consumerization of healthcare and how COVID accelerated the move to digital patient-centric health, the importance of “forever transaction” in treating patients, and the challenges of developing a clear business model in a highly complex environment.
—
Listen to the podcast here
Midi Health’s Joanna Strober on the Ultimate Forever Transaction—Healthcare
My final guest of season three, Joanna Strober, was the very first guest on the show. Back then, we were talking about Kurbo, the children’s service for WW. That’s Weight Watchers’ new name. She’s back to talk about her latest venture in direct-to-consumer healthcare, Midi. While Kurbo focused on helping kids get to and maintain a healthy weight, Midi is for women in midlife helping them get better as they get older.
You may have noticed my interest in how the way we stay healthy is changing, with guests from WHOOP, Thirty Madison, and Strava this season alone. I am fascinated by all of the transformations in the space as organizations embrace the concept of a Forever Transaction. After all, what forever promise is more compelling than more happy, healthy minutes?
Watch the space. Healthcare is embarking on a massive rethinking of how to better align its business models with patient outcomes. Midi is a great example of this. In our talk, we’ll cover the consumerization of healthcare and how COVID accelerated the move to digital patient-centric health, the importance of forever transactions in treating patients, and the challenges of developing a clear business model in a highly complex environment.
—
Welcome back to the show.
Thank you. I’m excited to be here.
It’s so great to have you back. I know we want to talk about Midi, the new company that you’ve launched, but before we get there, I want to catch people up. When we last talked to you in January of 2020, you were leading Kurbo, part of WW, the company formerly known as Weight Watchers. A lot has happened since then. Can you catch us up?
Yeah. We sold Kurbo to Weight Watchers in 2018. I spent two years integrating Kurbo within the overall business, growing the team, and figuring out how to integrate it into the overall organization. After being there for two years, I promoted a number of people within my organization and decided that I was interested in pursuing other entrepreneurial ventures.
You’re always the entrepreneur at heart.
I like to solve problems, so it’s always fun to think about new problems to solve.
Tell me about Midi and the new problem that got you thinking about diving back in and starting a new company.
Midi started with some emails to friends right around the time you and I talked in January of 2020 where we were commiserating about not sleeping, the other challenges that were happening in our bodies and not understanding what was happening. Why we were all wide awake at 3:00 AM, or having anxiety attacks or migraines and gaining weight. There were all these crazy things were happening to people that I knew. We weren’t getting good care, so that sent me down this rabbit path. We’re trying to understand how we could get people better care and what it would take to make that happen.
What I learned is that part of the why we weren’t getting good care is there are not enough trained doctors. Only 20% of OB-GYNs get any training in menopause. People go to become OB-GYNs because they want to deliver babies. There are not enough practitioners of women to help women in midlife after their fertile years, so the goal was how could we get more knowledge, how could we scale more expertise, and how could we create a company that would help women through the next period of their life.
D2C Healthcare: Medical professionals don’t actually look at this as a competition. They look at it as a way that they can focus on what they’re good at.
We’ve talked last time about this concept of a forever promise that if you want to have an ongoing relationship with your customer, you need to make them a promise to solve an ongoing problem or help them achieve an ongoing goal. What do you think of the promise that you want to make to these women at midlife?
That’s such a good question because I think a lot about that. We really want to thrive during this time period. It’s not about just feeling better. It’s about feeling great. It’s about helping women age healthier, live healthier, and thrive during a pretty big period of time in their life. 40-plus is a long time. We want you to live the best life that you can during that time, and that’s what we’re here to partner with you to do.
It’s a lofty goal. As a woman in that age range, it’s one that feels personally important. There are lots of hormone changes happening in your 40s, 50s, and beyond, and that does have a huge number of health issues that a lot of women power through.
They’re told to just grin and bear it.
One of the things that I’m interested in is how you build a model. If you want to help women to thrive from this point on, which is as you said, a long time, how do you think about the way you design your business model and the offering that you put forward to your members? I don’t know if I can even call them members, customers, or patients. What’s the right term?
When you’re a practitioner talking to our person, they’re a patient, but we want you to feel like you’re a member of our organization, so we do believe that you’re both a patient and a member when we think about our value proposition to you. What happens during this period of time is maybe you’re like me, you’re around 46 and you stopped sleeping. A few months later, maybe anxiety attacks start, or a year later, you have brain fog. All of a sudden, you don’t remember where your keys are or you’ve lost your car in the parking lot. We want to be the place that you come back to as new symptoms emerge, so what we’re thinking of this is that we think of it as iterative care.
You’re going to come to us and we’re going to help you with one problem. We’re going to get to know you. We’re probably going to have some blood testing and maybe genetic testing, and then, we’re going to have this big data set. You’re going to come back and we’re going to help with the next problem and the problem after that. We will also look at what supplements or medicines are you taking and how can we evolve those as new symptoms come up. Our goal is to be your partner during these periods of time when your hormones are fluctuating. They’re going up and down and crazy things are happening. It’s how can we partner with you during that entire process and be the trusted source for help.
First of all, that’s an interesting point about when you’re with your physician, your nurse practitioner, or your medical care provider, you’re a patient, but in the context of Midi, you’re a member, and membership has implications of longer-term and ongoing relationship as does patient, although a patient implies that you’re needing treatment, whereas member has some different connotations. Nomenclature is challenging for a lot of organizations to figure out what words do we use and what do they mean internally to us to help our team think about the people they serve in the right way and also how do those words land with the people we serve.
We went back and asked all of our pilot patients this exact question. We were like, “Do you want to be a patient? Do you want to be a member? How could we make you feel most comfortable?” It was from our conversations going back and talking to them that when they were talking to the practitioner, they were a patient and they wanted that relationship. The relationship with Midi of how we provide education to them, how we recommend the right supplements to them, or how we invite them to join us in group coaching sessions would be a membership model. We have thought a lot about how we talk to people and make them feel most comfortable, and the feedback that we’ve gotten was this is the right approach.
What does it mean to be a member versus being a patient? As they say at AmEx, membership has its privileges. What does it mean to be a member? Is there a financial arrangement? Is there a data-sharing arrangement? What makes one person a member and another person not a member?
We think there are two parts to this. Part of it is building a community, and we’d like you to be a member of that community. We’d like you to want to share information about your symptoms with our community so we can use machine learning over a large group of people to give better protocols, give better care, and tailor people’s care much more broadly than just around you, but around helping the world of women to get healthier.
There’s not much research done on women in this age category, and our goal is to change that and to have a lot more research available on what works for this, and for that, be a member of our community to help us to solve these problems together. On the other hand, when you come to talk to your doctor, that’s much more of the patient’s relationship.
We believe that you’re both a patient and a member when we think about our value proposition to you. @joannastrober Share on XTo be clear, you can be a member of Midi and have access to community data and potentially even have direct relationships even if you’re not a paying patient.
Being a member, you can attend our seminars, come to our lectures, and participate in discussion groups. There are all sorts of things you’ll be able to do as a member of our community, and then your insurance company will pay for the services.
I’m trying to keep up because there are so many things that you’re bringing up that I want to dig into. The first one is the concept of membership. One of the things that I think about a lot is that membership, in many cases, has three components, not always, but often, which are, content, community, and what I call commerce. It’s transactional or exchange of specific services or products.
Content could be articles, seminars, webinars, or access to a database, and then, the community is people that you can talk to, write to, and chat with online for the feeling of not being alone. It sounds like you’re weaving all three of those together with the patient being a little more like what I would call commerce, although that’s not the right word here. Content is the aggregated data and then maybe community is the opportunity to interact with other individuals that have raised their hand and said, “I want to share what I’m going through,” or, “I want to ask a question.”
Part of the content is also we have access to amazing expertise. For example, we’re working with Dr. Mindy Goldman who’s the expert in survivorship at UCSF and she’s going to be joining us to help train our practitioners.
What is survivorship?
They’re women who had breast cancer or who had a high risk of breast cancer. There’s a lot of concern about the fact that when you have cancer treatments, it puts you into early menopause. Most doctors are scared of taking care of those patients because they don’t have the right level of training. What we’re going to be doing is training all of our practitioners on that, but also having talks and support groups on our website for women who are going through this. We think of it as both an opportunity to offer support, guidance, and education, and then also to have one-on-one visits with practitioners to discuss these issues.
Membership is a model that I believe in. It’s this idea of focusing on an ongoing problem, facing a group of people, knowing that group really well, and continuing to evolve the offering to meet their ongoing needs. In the case of healthcare, I think you know that I had someone from Thirty Madison on the show. There’s a whole rise of digital health companies that are focusing on specific chronic health issues. This is about a big transformation in the business model, moving from the traditional healthcare system to looking at the health of the patient through a different lens and approaching it with a different kind of treatment, not just patient care but also member care, to use your distinctions there.
What is the feedback you’re getting from people in the old world? Healthcare is a huge industry. What do practitioners say? What do administrators say? What do researchers say? How is that part going? I would imagine that people might go to their current practitioner and say, “What do you think of Midi as a solution to help me deal with my inability to sleep, my anxiety, and my hot flashes?”
Most people that we’ve talked to are excited because they know that there’s a lack of care in this category. If you try to go to Stanford for a visit on most of these symptoms, for example, it’s a nine-month waiting list in order to get in, and that’s common all throughout the country. There are not enough trained practitioners. People don’t look at this as competition. They look at it as a way that they can focus on what they are good at, which is usually delivering babies, for example, if you’re an OB-GYN or doing procedures and using us as a way to take care of this other type of symptom that requires expertise but doesn’t require in-person care.
Fifty percent of all counties in the United States do not even have an OB-GYN. It’s not like we’re going into this competitive business and saying, “We’re going to be taking away your patients.” Instead, there are way too many patients and there’s no place for them to go. We’ve also been talking to large medical institutions about doing relationships with them where they refer people to us with this type of issue and then we refer people back to them for mammograms, DEXA scans, ultrasounds, and all the other things that people need that do require in-person care.
Quite honestly, if you look at care in five years, I believe that most care will be done through telehealth and expertise that’s scaled through telehealth. You’ll go to hospitals or in-person practitioners for procedures, but the rest of the care will be given online. The insurance change is also what’s enabling this because, for the first time, you can get reimbursed for these visits online. That’s enabling an entire business model that you couldn’t have had a couple of years ago.
I imagine people that are reading this might be wondering why there is so much happening in the telehealth space. Can you say a little bit more about some of the changes that have happened in the last few years that have allowed for this acceleration of digital health?
D2C Healthcare: In five years, most care will be done through telehealth and expertise that’s scaled through telehealth. You’ll go to hospitals or in-person practitioners for procedures but the rest of care will be given online.
Yeah. Specifically, with regard to reimbursement and telehealth, the COVID regulations enabled you to get reimbursed for an online visit in the same way that you would get reimbursed for an in-person visit. Prior to COVID, that wasn’t possible. There were telehealth providers, but they had to get reimbursed outside of the insurance system with separate contracts. Now, if you are a practitioner, you can get reimbursed the same way online as you would in person. What this enables is for practitioners to get licensed in multiple states and then to get reimbursed for care across multiple states so you can truly expand healthcare businesses in a way that a few years ago, you would not have been able to do.
I believe you’re going to see national healthcare brands in the next few years. You’ll see a cardiovascular care brand, and you’re already seeing mental health care brands that are national. A couple of years ago, none of that was possible. This change in laws has enabled a new type of health care company to emerge which they can scale expertise in a way that has never been seen before. Someone like Dr. Goldman at UCSF, now, we can license her in multiple states. We can use her to develop protocols that are unbelievably sophisticated for people who had cancer, and that we can scale access to those protocols nationally and get reimbursed by insurance for those visits. You could never have done that until recently.
One of the things that are coming to mind, which I know is a little crazy, is what the ride-sharing companies did to New York City medallions. There weren’t enough taxis. The taxis weren’t there when you needed them. They weren’t always clean and didn’t always feel safe, and then suddenly, this whole new group was allowed in and it changed the way that the whole system worked.
It sounds like you’re pretty optimistic about it not just for the health of women in midlife, but also for cardiovascular care, mental health, and all different categories. What are some of the challenges in being one of the early people on the frontier of this new way of treating patients, and what’s different maybe from the challenges at a place like Kurbo or even at other organizations that you’ve been involved in with in the past?
It doesn’t mean that because this has been opened up, it’s easy. To be clear, the licensing requirements are still on a state-by-state basis, so you still need to go state-by-state to get your practitioner’s license or nurse’s license.
What does that mean? What does that entail?
It’s a nine-month process per state and it’s expensive, so to set up an infrastructure like this, there are a lot of costs that you might view as unnecessary. Of course, the states control healthcare for a lot of reasons and it’s not going to be a national business. The conflict is that states license the practitioners. There’s no national license, so to build a national business, you still have to go state-by-state. It’s expensive and time-consuming, but it’s now possible. Before, it was not possible.
I’m also not going to tell you that billing is easy. It’s another complicated process. I would say the one thing I’ve learned a lot about billing insurance companies, and I understand why so many sole practitioners go out of business, is a lot of work to put in these billing infrastructures. Large organizations can hire huge teams of people to do that, which is what we are doing. It’s hard to be a sole practitioner because there’s so much overhead that goes into building these billing systems. We can now build a national business that does this, but it’s hard to do that as a sole practitioner.
An interesting thing to think about or something that I think about is that when I work with subscription businesses that are consumers like WW, the only person that has to decide to pay is me. I pay you and the organization thinks, “Do we let her do credit cards or other forms of payment? What are the forms of payment that we’re going to allow for her?” It’s quite simple.
Going either B2B or through a wholesale distributor is one level more complicated where you’re thinking about what kind of discounts do we give if you buy it through a channel partner, for example, or if somebody is buying it on behalf of a bunch of people like you sell into a university or company. This is a whole different level because every individual that comes to you directly has a financially complex picture, like this kind of insurance or these kinds of conditions living in this state.
Each practitioner has a complex situation in terms of where they’re allowed to practice and what their expertise is, and there are all kinds of legal and regulatory complexity that some of which is there to protect us and some of which are there for historical reasons because that’s the way it was built. There’s a lot going on in the healthcare space if you want to get into this. I want to say that just because it’s hard for you as the company does not mean it should be complicated for the consumer.
There are two parts. One is there are a number of companies that have emerged to help you do this so we don’t have to do this all ourselves. A few years ago, we probably would have, but now, there are companies that have emerged specifically to help digital health companies do these types of things. There are billing companies and also licensing companies.
We have an iterative process with you to help you feel better. The more you tell us about what is working and what isn’t, the more we’ll be able to change what we’re doing to respond best to your body. @joannastrober Share on XWe’re working with a whole host of really good companies that are helping us do this and that is enabling us to scale each of the different parts of this business so we don’t have to do it on our own. We wouldn’t be able to do this. We’ve set up the whole thing in about nine months. It would have taken three years previously to try to do something like this. Now, there are a lot of APIs that are available and you can connect to a number of other systems that enable this to happen.
Let’s be clear. You have a great team at Midi, but this is not anywhere near the scale of WW. This is a small team of people that are working towards national presence and licensing all these people. It’s a relatively small team that you have.
We expand our team by working with a lot of other partners that help us to scale faster.
As we record this, you’re days away from launching. What is it going to look like at launch? What can people expect and who’s eligible? Who is this for in the early days?
We’re launching only in California. We have insurance contracts with all the major companies in California, so if you have a California PPO, most likely, you will be a potential patient or member of ours. We are working to get more contracts as we speak. You can also do cash pay visits, so it’s not only insurance. If someone wants to pay cash, that’s great, but we will have all the insurance companies set up in California, and then we’re going as fast as we can. We should be in 30 states by the end of 2022. You can come to us. We have a long onboarding process where we learn a lot about you, the different symptoms, and your family history.
Let’s say you launch. I live in California, I’m 40, and I’m noticing some symptoms or some things where I don’t feel like I’m at my best anymore and I’m not sure why. I reach out to you, and then what happens? How do I know if I’m a good fit and what can I expect if I’m used to only being a patient when I physically go to my doctor’s office?
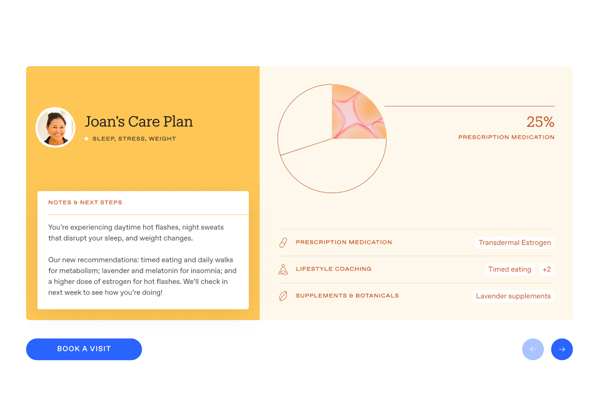
It’s similar to going to a doctor. You’ll book an appointment with us and tell us what your symptoms are. Instead of going in person and having to fill out a long questionnaire about your symptoms, you’ll do it all online. Our doctors then have access to all of that information. They will see everything that you put in there. You will have a visit with a practitioner and they will probably send you to get a blood test or a saliva test on what’s appropriate maybe for your hormone levels, thyroid, Vitamin D, or whatever else is appropriate for you. You will then come back for another visit and we will tailor treatments to you.
We will either recommend prescription medicines or supplements. We will facilitate getting those to your home and then you will report back to us on your symptoms and how they’re resolving. You will come back to us in a few months to help us to continue to titrate and iterate. We think of this as an iterative process with you to help you feel better. The more you tell us about what is working and what isn’t, then we’ll be able to change what we’re doing to respond best to your body.
I make my appointment, I fill out a questionnaire online at my convenience, and my practitioner looks at that before they meet with me. We have a conversation and go through all of the symptoms I’m feeling and maybe, they have me do some tests or get additional information. We come up with a treatment plan, and then you said that I report back. Does that mean somebody calls me?
It’s all done via text. One thing we care deeply about is tracking that data, and we won’t be able to track the data if it’s on phone and you just tell us the symptoms. We need you to come back to our site and give us numbers if you have improved from X to Y to Z so that we can track outcomes appropriately. We care a lot about collecting this data so that we can have treatments for everyone to be more effective.
This is important for people that are reading. One of the big things around building a forever transaction with customers or our members is the ongoing engagement. I can imagine why somebody would come to you not being able to sleep, not being comfortable, or not being able to do work. You get whatever is prescribed or whatever kind of treatment and recommendations are made. Do you reach out to me to get me to come back and give you feedback? Do you schedule another meeting? What is the kind of cadence that I might expect?
For a long time, I’ve heard other people at your organization refer to the symptoms as whack-a-mole. You solve the sleeping problem, but then suddenly, you’re having the hot flashes or you solve the hot flashes and suddenly, you have brain fog. Can you talk to us a little bit about the engagement piece and how you keep people making this into a habit and allowing you to continually improve their experience and that of the other people that are part of your larger community?

D2C Healthcare: I believe you’re going to see national healthcare brands in the next few years. You’ll see a cardiovascular care brand and you’re already seeing mental health care brands that are national. A couple of years ago, none of that was possible.
We will be reaching out to you for feedback. The visit cadence seems to be most appropriate quarterly. There’s a lot of titrating involved.
What is titrating?
It’s changing the dosage. You might come to us and be very open to hormone replacement therapy and want to try the patch. There are three different types of patches. You’ll try one patch and then see how you’re feeling. You’ll then come and say, “I’ve changed my mind. I’d like to try the gel and see if that improves my sleep a little bit more,” so we’ll maybe change it to the gel or maybe try a pill.
It is not one size fits all. There are lots of different approaches that work for women, and it takes a lot of iterating, titrating, and testing to see what works best. We might also say, “Maybe you should try the estrogen at night and the progesterone in the morning,” to give you examples, or, “You’re having some anxiety. We have this amazing cortisol manager that is a supplement that includes L-theanine and ashwagandha. Why don’t you try to take that in the evenings and see if that helps you with your hot flashes?”
There are lots of different approaches. We have a combination of functional medicine and traditional medicine and we’re able to try both. We will help you to figure out what is most appropriate for you. If you’re sleeping through the night, that’s great. If you are not sleeping through the night, let’s have another visit and try something else.
I could talk to you for hours about this, and honestly, we have and we probably will. We’ll continue. I’m a huge fan of what you’re doing as an investor, a professional, and a personal woman in midlife who wants to feel her best every day. Before I wrap up this conversation, are you up for a speed round like we did the first time?
Yeah.
The first question is what is your favorite health hack?
Recently, it’s the cortisol manager. I really think it calms my mind and helps me to sleep better.
What’s a lasting habit from your work with Kurbo?
It’s keeping track of healthy and unhealthy foods so that I don’t get stressed about what I eat.
What is the best subscription your startup is using to run the business?
It is not a one size fits all. There are lots of different approaches that work for women and it takes a lot of iterating and titrating and testing to see what works best. @joannastrober Share on XWe are using a lot of subscriptions to run this business. I don’t know if I have a good example for you about that, but maybe Medallion, which is helping us to get our people licensed in all 50 states and keeping track of each of their eligibility to work in each state and then helping us also to get these insurance contracts in each state. Medallion is addictive for us.
I’ve never heard of it. I’ll have to look into it. What is the most surprising thing you’ve learned about health in midlife?
Estrogen for most women is the fountain of youth.
Here’s the final question. For people that are reading this who are like you and are entrepreneurs in consumer health, digital health, or telehealth, what would be one tip that you would give them to keep in mind as they launch a new way of providing healthcare?
I believe that the consumerization of healthcare is just the beginning. Consumers in the end are going to make the decisions, so the most important thing is do you have an experience that consumers like, trust, and respond to emotionally so that they feel like you’re taking really good care of them? I do believe that over the next 5 to 10 years, we’re going to have consumer brands that focus on healthcare, and the companies that are going to win there are going to be the ones that are creating a great consumer experience for their patients.
I’m always fascinated to talk to you. Thanks so much for being our first guest and also our first guest to make a second visit. I appreciate spending time with you.
Thank you. This was fun. I enjoyed it.
—
That was our final guest of season three, Joanna Strober, Founder and CEO of MIdi. For more about Joanna and Midi, go to JoinMidi.com. Also, if you liked what you read, as always, please go over to Apple Podcasts or Apple iTunes and leave a review. Mention Joanna and this episode if you especially enjoyed it. We read all the reviews because we want your feedback.
We’ll be back next season with more subscription stories. In the meantime, check out some of our most popular episodes including those featuring Mighty Networks’ Gina Bianchini, product expert, Elena Verna talking about the role of freemium, and Tinder CEO, Renate Nyborg, on going global with your subscription model. Thanks for your support and thanks for reading.
Important Links
- Joanna Strober, Founder and CEO of Midi
- Midi
- Subscription Stories Episode with Ben Foster of WHOOP
- Subscription Stories Episode with Matthew Mengerink
- Subscription Stories Episode with David Lorsch of Strava
- Subscription Stories Episode with Joanna Strober
- WW
- AmEx
- Dr. Mindy Goldman
- Stanford
- Medallion
- Robbie Kellman Baxter
- Subscription Stories: True Tales From The Trenches on Apple Podcasts
- Subscription Stories Episode with Elena Verna
- Subscription Stories Episode with Gina Bianchini
- Subscription Stories Episode with Renate Nyborg
- Mighty Networks
- Tinder
- Forever Transaction
About Joanna Strober
 Joanna Strober is the CEO of Midi Health, the only virtual-care platform for women 40+ covered by insurance. Prior to Midi, Joanna founded Kurbo Health, a digital therapeutic for childhood obesity that she grew to serve tens of thousands of adolescents worldwide and sold to WW in 2018.
Joanna Strober is the CEO of Midi Health, the only virtual-care platform for women 40+ covered by insurance. Prior to Midi, Joanna founded Kurbo Health, a digital therapeutic for childhood obesity that she grew to serve tens of thousands of adolescents worldwide and sold to WW in 2018.
Prior to following her passion for digital health, Joanna spent fifteen years making investments in venture capital and private equity. Joanna is also the co-author of Getting to 50/50, a best selling book written to help parents thrive in the workforce after having children.
Love the show? Subscribe, rate, review, and share!
Join the Subscription Stories Community today: